Medicine is on the verge of a revolution, and its name is bioprinting.
A technology that, until recently, seemed like science fiction is now saving the lives of millions of people in need of organ transplants. Yes, we are talking about those same 3D printers that could once print plastic toys and figurines at most. Today, they print tissues, vessels, and even entire organs, thereby opening up unprecedented opportunities for medicine to treat the most complex and life-threatening diseases.
The History of Bioprinting: From Ink to Living Cells
The history of bioprinting is an exciting journey spanning several decades. It began in the late 1980s, when scientists began exploring the possibilities of 3D printing to create various materials (primarily for construction and engineering, and only then for everything else). Thus, the first 3D printer appeared in 1988 thanks to the efforts of Charles Hull, but, of course, it did not gain widespread use due to its high cost and imperfections.
It was only in the early 2000s that researchers took the first step towards bioprinting by creating a prototype printer capable of applying cells to various surfaces. At the same time, the concept of bio-inks emerged - a material combining living cells and special gels, which would provide them with support and nutrition. This period was marked by the beginning of experiments with the creation of simple tissues, such as skin and cartilage.
An important breakthrough was the patenting by Thomas Boland from Clemson University in 2003 of inkjet printing technology for creating cellular structures. This is the moment that can be considered the starting point of modern bioprinting. In subsequent years, bioprinting developed at a rapid pace, and new printing methods appeared, such as extrusion bioprinting, where bio-ink is extruded through a nozzle, and laser-induced transfer, where a laser is used to transfer cells to a given surface.
The 2010s became a period of active search for even more advanced, safe and convenient printing methods for medical purposes. Scientists began to print more complex structures, such as blood vessels and heart valves. In 2013, Organovo Holdings made a breakthrough by printing the first functional human liver. Although it was just a small fragment of tissue, it demonstrated the fundamental possibility of creating complex organs using bioprinting. And in 2019, the Russian company 3D Bioprinting Solutions printed the first functioning thyroid gland of a mouse, which was successfully transplanted to an animal, thereby confirming the operability of the technology in practice.
After 2020, what we have now appeared, namely, new bio-inks, which better support the viability of cells and ensure the formation of the correct biostructure. Now bioprinting allows you to print even more internal organs and, although it has not yet come to a complete replacement of donors, it is already actively used in the field of transplantation.
What Organs Can Be “Printed” in 2025?

Although creating complete, functioning organs for transplantation still remains a complex task, the technology is already demonstrating impressive results in printing small organs or tissues, since it is easiest to guarantee their engraftment. Thus, a 3D printer can create:
-
Skin. Printed skin is successfully used to treat burns resulting from fires, chronic wounds, ulcers, and other damage, providing rapid healing and reducing the risk of scar formation. For example, Renmatix has developed a skin printing technology that allows the creation of tissues identical to the patient’s skin, which minimizes the likelihood of rejection and, in addition, guarantees a good aesthetic effect.
-
Cartilage. Bioprinting of cartilage tissue opens up new possibilities for the treatment of joint diseases, such as arthritis and osteoarthritis. Poietis, using laser bioprinting, creates cartilage implants that not only fill defects but also stimulate the regeneration of the patient’s own cartilage.
-
Blood vessels. Creating functional blood vessels is a critically important step towards printing more complex organs. Printed vessels can be used to treat peripheral artery disease, for bypass surgery, and also to provide nutrition and vascularization to printed organs and tissues.
-
Heart valves. Bioprinting of heart valves is a promising alternative to traditional methods of treating heart defects, such as mechanical and biological valve prostheses. Printed valves, created from the patient’s own cells, can grow and adapt with the body, which is especially important for children with congenital diseases.
-
Liver. Although creating a complete liver for transplantation remains a complex task, bioprinting of liver tissue fragments (liver lobules) is already used today to test drugs and study liver diseases. For example, Organovo Holdings has developed a technology for printing 3D liver models that allow for more accurate assessment of the toxicity and efficacy of new drugs than traditional methods of testing on cell cultures.
Bioprinting also demonstrates successful results in creating small organs and tissues, such as the trachea, bladder, and individual fragments of the kidneys. These achievements open up new opportunities for the treatment of diseases of these organs and reducing the need for donors.
And yet, the main goal of bioprinting, for which all this was undertaken, remains the heart, since it is the most sought-after among the organs for transplantation. According to the World Health Organization, heart failure is one of the leading causes of death in the world. In the United States alone, thousands of people are on the waiting list for a heart transplant.
The complexity of bioprinting the heart is that the heart consists of various types of cells, including cardiomyocytes (heart muscle cells), fibroblasts (connective tissue cells), and endothelial cells (cells lining blood vessels). Nevertheless, scientists have managed to learn how to print heart valves and myocardial fragments, but there is still a long way to go before printing the entire organ.
What is needed to print organs? Biology, Science and Ethics
The bioprinting process is a complex and multi-stage process that requires the integration of knowledge from various fields of science, including biology, chemistry, engineering, and medicine. Each stage requires high accuracy, control, and understanding of biological processes:
-
Obtaining and preparing cells. Cells are obtained directly from the patient (to reduce the risk of rejection), and then used to create bio-inks. Stem cells are usually used, which can be obtained from bone marrow, blood (peripheral blood or umbilical cord blood), or other tissues, such as adipose tissue, for example. Stem cells, especially mesenchymal stem cells (MSCs), have the ability to differentiate into various types of cells (cardiomyocytes, chondrocytes, hepatocytes, etc.), which makes it possible to create tissues and organs with the required structure and function on their basis.
-
Creating bio-inks. Prepared cells are mixed with a special gel – a biomaterial that provides support, nutrition and the correct location of cells in the printing process. The composition of bio-inks is selected individually for each type of tissue or organ, taking into account the needs of cells in nutrients, growth factors and other biologically active substances. The gel should also have certain physical properties, namely viscosity, thixotropy, the ability to quickly harden after printing, to ensure the preservation of the shape of the printed structure. At the same time, it is very important that the biomaterial is decomposable and dissolves in the patient’s body without harming him after transplantation.
-
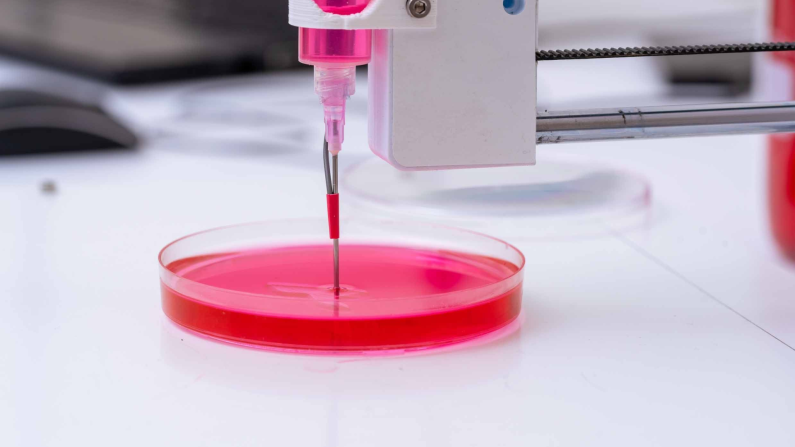
Printing. Bio-inks are loaded into a 3D printer, which applies them layer by layer to a given surface, creating a three-dimensional structure of an organ or tissue. There are various bioprinting methods: inkjet printing, extrusion printing, laser-induced printing, and others. Each method has its own advantages and disadvantages in terms of accuracy, speed, and cell viability. The printing process is controlled by a computer, which uses data from computed tomography (CT) or magnetic resonance imaging (MRI) to create an accurate three-dimensional model of the organ to be replaced or restored. At the same time, it is important to monitor the condition of the cells during the process so that printing does not accidentally cause their death.
-
Maturation and vascularization. After printing, the organ or tissue is placed in a special bioreactor, where the conditions necessary for maturation, the formation of functional tissue and vascularization (the formation of blood vessels) are created. The bioreactor provides optimal temperature, pH, oxygen concentration and nutrients, as well as mechanical stimulation, simulating the natural environment of the body. Vascularization is a critically important stage, since blood vessels provide nutrition and oxygen to all cells of the printed organ, and also remove metabolic products.
Risks and Dangers of Bioprinting

Like any breakthrough technology, bioprinting, despite its colossal prospects, carries a number of risks and potential dangers, primarily, of course, for the patient, for whose sake these technologies are applied.
So, one of the main problems remains the risk of rejection of the printed organ by the patient’s immune system. Our body, recognizing foreign cells, automatically launches an autoimmune process aimed at destroying the implant. To minimize this risk, scientists use the patient’s own cells to create bio-inks. However, even in this case, rejection is not excluded, since the process of cultivation and printing can change the surface cellular antigens. Research in this area, for example, the work of Professor Anthony Atala’s group at the Wake Forest Institute for Regenerative Medicine, is aimed at developing new methods of immunomodulation and creating biocompatible materials that can reduce the human immune response after the transplantation of a printed organ.
Another serious problem is the risk of infection. The process of printing and maturation of the organ requires strict adherence to sterility. Even slight contamination can lead to the development of an infection, which will endanger not only the viability of the printed organ, but also the patient’s life. Research in the field of antimicrobial bio-ink development, for example, the work of Professor Ali Khademhosseini’s group from the Harvard Medical School, is aimed at creating materials that can prevent the growth of bacteria and other microorganisms.
One should not forget about the potential toxicity of the materials used to create bio-inks. Gels, polymers, and other additives can have a negative impact on cells, disrupting their function and viability. Therefore, scientists pay special attention to the development of biocompatible materials that do not cause inflammation, toxic reactions, and do not interfere with cell growth and differentiation. Research in this area, for example, the work of Professor Mark Skylar-Scott’s group from the Massachusetts Institute of Technology, is aimed at creating new generations of bio-inks based on natural materials, such as collagen, fibrin, and alginate.
Finally, bioprinting also poses serious ethical questions to society. The creation of artificial organs, manipulation of genes, and the possibility of “improving” the human body - all this requires careful discussion and the development of clear ethical rules. For example, the question of the availability of bioprinted organs and tissues, especially in the early stages of technology development, can lead to social inequality and discrimination. In addition, the possibility of creating organs with improved characteristics raises questions about the boundaries of intervention in human nature and the potential consequences for evolution.
And at the same time, the possibilities and prospects of bioprinting are too wide to be abandoned. It can be used not only for donation, but also for creating models for teaching medical students, which is especially important for complex medical areas, such as neurosurgery. In the future (very distant, of course), this can hypothetically allow the creation of bioimplants and prostheses for people who have lost limbs. Imagine transplanting an entire arm, alive and functioning! In 2025, we can only observe the beginnings of future technologies that will undoubtedly once completely change human life - and, without a doubt, for the better.
Share this with your friends!




Be the first to comment
Please log in to comment